- What is Neurogenic Bladder?;
- Is there Neurogenic Bladder without a neurological disease?
- How is Neurogenic Bladder classified?
- What are the symptoms in Neurogenic Bladder?
- How is Neurogenic Bladder classified?
- What is the treatment of Neurogenic Bladder?
What is Neurogenic Bladder?
Neurogenic Bladder is a general term describing urinary disorders in patients with established neurological disease. Among others, such cases are patients with multiple sclerosis, Parkinson's disease or spinal injury presenting urinary incontinence or inability to urinate. Neurogenic Bladder may also include urinary disorders that are due to non-neurological diseases, which may though gradually cause severe impairment to the nervous system. For example, patients with chronic diabetes mellitus may have established diabetic neuropathy resulting in neurogenic bladder and urinary disorders.
Is there Neurogenic Bladder without a neurological disease?
Only in rare cases will patients with no established neurological disease present symptoms and urological findings similar to those of neurogenic bladder. This rare entity of ' Non-Neurogenic Neurogenic Bladder' is elsewise called 'Hinman syndrome'. The full etiology of this syndrome is unclear. However, it is known today that urinary disorders may precede months or even years before the diagnosis of a neurological disease. A probable cause of Hinman syndrome could be of psychological origin (psychogenic urinary disorders)
How is Neurogenic Bladder classified?
The simplest and easier way to classify the condition of Neurogenic Bladder is to distinguish it in 'Spastic Bladder' and 'Atonic Bladder'. In Spastic Bladder, the main disorder is the contraction of the bladder, which is uncontrollable by the patient (involuntary). On the contrary, in Atonic Bladder there is total absence of bladder contraction. The severity of Spastic Bladder varies from patient to patient. In the most severe cases, there is high risk for renal failure. The likelihood for renal impairment is significantly limited in Atonic Bladder, even though the patients' quality of life is critically affected by the inability to urinate and urinary incontinence.
What are the causes of Neurogenic Bladder?
Almost all neurological diseases are potential causes of Neurogenic Bladder.
Such diseases are:
- Multiple Sclerosis
- Parkinson's Disease
- Multiple System Atrophy (MSA)
- Cerebrovascular Accidents (Strokes)
- Congenital Spinal Cord Diseases (Meningomyelocele)
- Traumatic Spinal Cord Injuries
- Severe Spine Discopathy
Yet, there are a great number of other medical conditions and diseases that may be involved in the Neurogenic Bladder etiology.
What are the symptoms in Neurogenic Bladder?
Patients with Neurogenic Bladder manifest a variety of urinary symptoms that cause discomfort and affect their quality of life. These are symptoms related to the filling of the bladder (urinary frequency, urgency, nocturia, incontinence etc), as well as symptoms occurring during the actual process of micturition (full inability to urinate, difficulty in urinating, sensation that the bladder never empties etc).
How is Neurogenic Bladder diagnosed?
The initial evaluation of urinary disorders in Neurogenic Bladder includes the patient's detailed history and clinical examination. Then follow basic laboratory blood tests and simple imaging screening (e.g. urinary tract ultrasound). The assessment is usually completed with invasive urodynamic tests, such as Flowometry. As long as it is considered necessary by the physician, the patient may undergo more specialized invasive urodynamic and imaging tests performed by expert Neurourologists.
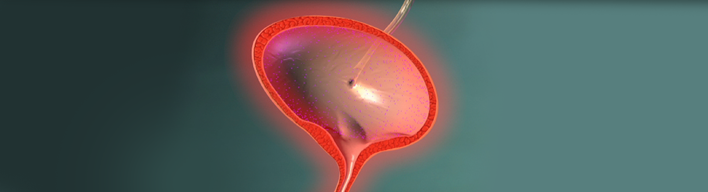
What is the treatment of Neurogenic Bladder?
Once the urinary disorder is diagnosed, the treatment aims at protecting the patient from major complications. The physician's prior objective is to protect the patients' renal function, improve their quality of life by providing full cure or, at least, by mitigating significantly urinary symptoms.
The treatment of Neurogenic Bladder varies from case to case, depending on the severity of the urinary disorder, the patient's expectations/desires and his/her neurological condition. It is imperative to provide thorough information about all therapeutic options, explaining both advantages and disadvantages of each one of them.
More specifically, treatment options may include:
- lifestyle changes, concerning mainly adaptation/regulation of liquid intake during the 24-hour period
- pharmacotherapy, aiming mainly at reducing "bladder spasticity" and limiting incontinence
- full voiding of the bladder at regular intervals with the use of intermittent catheterization (single-use catheters)
- combination of all the above
In case the above therapeutic options are not effective, there are less or more invasive therapies that could be recommended, such as bladder Botox injections, urethral infusion of dilatant fluids, a neurostimulator (bladder 'pacemaker') placed in the spine and surgical interventions for increasing the size of the bladder.