- What organs does the urinary tract consist of?
- What are the functions of the urinary tract?
- Anatomy of the kidneys
- Functions of the kidneys
- Bladder and Urethra Anatomy
- What is the urine?
- How much urine is normally produced on a daily basis?
- How does the urine transfer to the bladder?
- What happens if the urine meets an obstacle on its way to the bladder?
- What if ureteral obstruction becomes permanent?
- How is the urine stored in the bladder and how is the process of micturition stimulated?
- How is micturition controlled?
What organs does the urinary tract consist of?
The urinary tract is composed of the 2 kidneys and 2 ureters (upper urinary tract) and the bladder and urethra (lower urinary tract). Kidneys are bean-shaped organs. Adrenal glands are endocrine glands that sit at the top of kidneys, produce hormones and do not belong to the urinary tract. The anus and rectum, i.e. the terminal part of the bowel, are located behind the bladder. Other organs bordering the bladder related to urinary disorders are the organs of the genital tract. In males, the prostate gland surrounds the urethra from the point the urethra meets the bladder. Seminal vesicles -producing seminal fluid together with the prostate- are adjacent to the posterior bladder wall and are both anatomically and functionally in close proximity with the prostate gland. In females, the vagina is located behind the urethra and bladder, while the uterus 'embraces' the bladder from back and below.
What are the functions of the urinary tract?
Urinary tract organs carry out the following functions:
- They produce urine with the help of kidneys - thus, restoring the body balance in water and vital substances for the regulation of blood pressure and blood production (i.e. haematopoiesis).
- They substantially contribute to waste removal from the organism, mainly of protein residues which are mostly nitrogen compounds.
- They actively transfer the urine downwards throught the pelvis, kidneys and ureters (=thin tubules terminating in the bladder).
- They store urine in the bladder.
- They discharge urine out of the body through the urethra by means of micturition.
Anatomy of the Kidneys
There are 2 kidneys (right and left). Both of them are bean-shaped organs, about 11-12cm in size (almost the size of our fist). They are located on the right and left of the spine -right below the thoracic cavity behind the peritoneum- and sit on the posterior abdominal wall. The right kidney is lower than the left one. Kidneys consist of the renal parenchyma (=glandular tissue producing urine) and the pelvis (=reservoir collecting urine to be promoted towards the ureters).
Functions of the Kidneys
The kidney functions as a compound tubular gland producing urine. The urinary tract -along with lungs, skin and bowel- removes from our body substances that are useless or harmful in our nutrition (debris). Kidneys, in particular, discharge all harmful waste through the urine they produce.
Kidneys also contribute substantially to a vital function called 'homeostasis', i.e. regulation of electrolytes and blood pressure. They are responsible for the reabsorption of water, glucose and aminoacids, all being substances essential for the smooth function of our organism.
In addition, kidneys produce some important hormones, such as renin (hormone determining blood pressure) and erythorpoietin (essential hormone for the production of red blood cells).
Bladder and Urethra Anatomy
The bladder is a hollow balloon-shaped muscular organ. In fact, it is a reservoir attached to the pelvis with ligaments that are connected with pelvic muscles and bones. These muscular and ligamentous structures compose the pelvic floor (= pelvic lower surface) upon which other organs 'sit', such as the bladder, prostate (in men), bowel and uterus (in women). That is the reason why it plays such a crucial role in urinary retention (control of micturition). Urinary retention is secured by the pelvic floor and a bundle of orbicular muscles, composing the sphincter that helps us control any potential urine leakage (urinary incontinence). Sphincter muscles tightly surround the bladder outlet towards the urethra. The urethra is a small tubule participating in the urine discharge out of the body. The female urethra is much shorter than in males (i.e. only 4cm), and that is why women suffer from urinary tract infections more frequently than men, as it is much easier for microbes to enter the bladder. It should be pointed out that the front part of the urethra always hosts some microbes, which, however, in normal healthy conditions cannot enter the bladder.
What is the urine?
Kidneys serve the body as a 'natural blood filter'. All toxins and metabolic waste (e.g. urea and ammonia) are carried away with urine. Urine is produced through the tiny filtering units called 'nephrons' that are located in the renal cortex. About 95% of the urine content is water. The urine has a pale yellow colour and the odor -determined by ammonia content- can be affected by the type of food consumed. The amount of urine output depends on many factors -particularly on the amount of liquids and food consumed, as well as the level of fluids discharged from the body by means of perspiration (sweating) and breathing. When the organism is dehydrated, the urine is dense and dark-coloured; on the contrary, when there is good hydration, the urine is light-coloured and more dilute. There are some pharmaceutical agents that can affect the amount of urine output. These are drugs that either increase urine (diuretics) or retain urine.
How much urine is normally produced on a daily basis?
This depends to a great extent on the amount of liquids consumed and the loss of fluids mainly by means of sweating and breathing. Thus, in summer -as there is more fluid loss from the body due to heat- the body produces less urine, in order to keep its balance. However, in adults the mean daily urine output ranges from 1 to 2 liters, depending on the liquids consumed. Polyurea (excessive urine production) is the condition when the urine output exceeds 2,5lt/day. On the contrary, Oligurea is the condition when the urine output is less than 400ml/day and Anurea when urine production reduces to even lower levels below 100ml/day.
How is urine transferred to the bladder?
Urine is produced in the renal parenchyma and initially accumulates in the renal pelvis, which is a kind of reservoir. As the pelvis contracts, the urine is directed towards two tubules called ureters, and transfers to the bladder. This process takes place spontaneously (passively), that is simply with the force of gravity. The muscles of the ureter walls make successive wave-like movements (alternate muscular contractions and relaxations); this phenomenon is called Ureteral Peristalsis and aims at forcing the urine to reach the bladder. Ureters are 25 to 30cm in length. Thanks to these peristaltic waves, small urine amounts empty into the bladder through the ureters almost every 10 to 15 seconds,.
What happens if the urine meets an obstacle on its way to the bladder?
If urine meets some obstacle on its way to the bladder (e.g. renal stone, ureteropelvic junction stenosis or blood clot in the case of hemorrhagic pelvic or renal tumour), then the kidney is dilated inducing pain, the known "renal colic". The colic is too strong and the patient cannot find a position to relieve the pain. As long as urine does not find a way to overcome the obstacle and unblock the passage, the colic remains. That is the reason why water should not be consumed at the time of the colic, in order to avoid increasing urine output in the kidney. On the contrary, once the obstruction is resolved and pain subsides, high liquid intake and urine production significantly helps to carry away sand or small stones to the bladder; from there these can remove more easily, for the urethra has a larger diameter than the ureters.
What if ureteral obstruction becomes permanent?
If the ureteral and pelvic dilation remains, this might cause an infection called Pyelonephritis, in which the kidney is gradually impaired due to the pressure exerted on it. The pelvis expands up to a certain point, the renal parenchyma gets thinner and damaged and ultimately the kidney turns into a non-functional sac containing stagnant urine. If both kidneys are blocked, then the patient will be led to renal failure -as happens in cases of bladder or prostate cancer where the two ureteral orifices (outlets of ureters into the bladder) are blocked. If something is not done immediately to unblock the kidneys, the patient will unfortunately end up to hemodialysis/ artificial kidney.
How is urine stored in the bladder and how is the process of micturition stimulated?
The bladder stores the urine and functions like a balloon that is slowly filling up. If the urinary tract is healthy, bladder capacity is about 400ml of urine, which is usually accumulated within 2-5 hours, always depending on the amount of liquids consumed. However, the first urge to urinate is felt when the urine concentration is 120-180ml. This initial urge will easily subside for it is only a simple warning. On the contrary, when there is more than 300ml, the bladder induces a persistent urge for micturition. When the urine fills up the bladder, we have an unpleasant intense sensation that forces us to stop any activity and run to the toilet. At this point, micturition becomes imperative. If we retain the urine for longer and it reaches 600 or 700 ml, then the bladder will contract and empty on its own for safety reasons; this is called spontaneous (automatic) micturition.
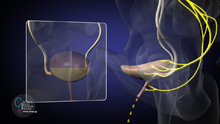
How is micturtion controlled?
The whole process of micturition is controlled by nerves -located in the bladder- and by the spinal cord -located in the spine- which send the message to the brain that the bladder is full. Thanks to this message we can sense when it is time to urinate. It is at that point that our urge to void our bladder gets more intense. When going to the toilet, our brain sends signals to the bladder muscles to contract and transfer urine from the bladder to the urethra. At the same time, the brain sends signals to the urethral sphincter to relax and in this way the process of micturition takes place in full coordination. When all these nerve signals are conducted in the proper order and there is harmonious coordination between the bladder and sphincter, then micturition takes place normally and the bladder gets completely empty. The spincter activates and contracts again right away, while the empty bladder automatically relaxes. This is a continuous cycle going on throughout our whole life! It should be pointed out that the sensation to urinate is not induced only by urine, but by any stimulus of the bladder. Thus, a bladder inflammation frequently induces the urge sensation to urinate, for the bladder is not 'smart' enough to distinguish among different stimuli.