- What is the Overactive Bladder Syndrome (OAB)?
- What is the incidence of the Overactive Bladder Syndrome?
- What are the causes of the Overactive Bladder Syndrome?
- What is the treatment of Overactive Bladder Syndrome?
- General lifestyle measures that may help
- Re-education of the Bladder
- Pelvic floor exercises
- Botox Therapy
What is the Overactive Bladder Syndrome (OAB)?
The bladder is overactive when there is a sudden urge for urination even if the bladder is not full. Overactive Bladder Syndrome is a common condition. The causes inducing these repeated and uncontrolled bladder contractions cannot be identified; for example, they are not due to a urinary tract infection or prostate dilation. Overactive Bladder Syndrome is also known as 'Spastic Bladder' or "Hyper-reflexive Bladder'.
The symptoms of the syndrome are:
- Urinary Urgency: sudden intense urge to urinate that cannot be inhibited and forces the patient to run to the toilet immediately
- Urinary Frequency: the patient urinates more than seven times during the day; in many cases, far more than that.
- Nocturia: the patient wakes up in the night due to urgent need for urination
- In some cases, Urinary Urgency may lead to Urge Incontinence, i.e. involuntary uncontrollable urine leakage and inability of the patient to make it to the toilet (wetting)
What is the incidence of the Overactive Bladder Syndrome (OAB)?
According to two large studies, about 1 out of 8 adults manifest OAB symptoms. Symptoms may vary as for their severity. Approximately 1 out of 3 patients with OAB also report some urge incontinence episodes. Although OAB is common in both men and women, urinary incontinence occurs more frequently in women.
What are the causes of the Overactive Bladder Syndrome?
The etiological mechanism of the syndrome is not yet fully known. The bladder muscle becomes oversensitive to the presence of urine and contracts strongly even if the bladder is not very full with urine. In normal conditions, the bladder muscle (detrusor) is loose during the whole time the bladder fills up with urine. When the bladder is half full, the bladder gradually stretches and makes us sense a first desire to urinate. Most people can control this sensation quite easily for some time before going to the toilet. However, in patients with OAB the bladder muscle seems to send wrong messages to the brain. The bladder contracts too early without warning, even though not being full. The patient feels an urge to urinate, which is characteristic in OAB. Recent data have shown that there may be some problem in the process of how the brain perceives or filters and intercepts the feeling of bladder fullness; this problem results in inability to control urination. The syndrome occurs more frequently as age advances. Also, symptoms may become more intense during periods of high stress and due to malnutrition (tea, coffee, soft drinks, alcohol).
In some cases, OAB symptoms emerge as complications of a disease, e.g. in patients with multiple sclerosis, cerebrovascular accident (stroke), Parkinson's disease or after spinal cord injury. In these patients, the normal communication of the bladder nerves with the brain and spinal cord (controlling urination) is interrupted and, as a result, they develop overactive bladder of neurogenic etiology. Also, similar symptoms may emerge in urinary tract infection, lithiasis or bladder cancer. In these cases, it is not characterized as overactive bladder syndrome, for the etiology is known.
What is the treatment of the Overactive Bladder Syndrome?
There are various therapeutic options, such as:
- LIfestyle changes
- Re-education of the bladder - pelvic floor exercises
- Pharmacotherapy
- Surgery
- Nerve Stimulation therapy (Neurostimulation) or Botox treatment
General lifestyle changes that may help
- In case there is no easy access to the toilet, this problem has to be resolved. Particularly in patients with motor problems, the place has to be properly arranged.
- Coffee, tea and soft drinks may aggravate symptoms. Try to give up or at least cut down on their consumption. Once you realize the condition improves, it is then up to you whether you avoid them as a lifestyle change. You should know that cafein, in particular, has high diuretic action -in other words, increases urine output.
- Alcohol may aggravate symptoms in some people. Follow the same recommendations as mentioned above with coffee consumption.
- Consume normal amounts of fluids; neither too little not too much. You may probably think that if you eliminate completely the amount of liquides consumed, your bladder will not fill up so quickly. However, this may even aggravate symptoms because the urine will become then more dense and cause irritation to the bladder. The normal amount of fluids is about 6-8 glasses of water/day, which should increase when the weather gets hotter.
- Go to the toilet only when necessary. Some people have the habit of going to the toilet more often than they really need to. If you go to the toilet too often, the bladder learns to retain only a little urine.
Re-education of the Bladder
The aim is that the bladder learns gradually to stretch in such a way that it is able to fit larger amounts of urine. With time, the bladder muscle becomes less and less overactive and you will be able to control more and more your desire to urinate. An expert physician or physiotherapist will explain to you how to e-educate your bladder. You will be given advice like the following:
- First of all, keep a urinary diary. In this diary you will note down the time each micturition takes place and the amount of urine. Also, note down the amount of liquids you consume and the exact time. It is important to note down any occurring incontinence episodes. The diary will be given to you by your physician and s/he will explain to you how to fill it in. It is a very useful tool for your physician in order to prepare a bladder re-education program that is tailor-made for you.
- The physician will recommend increasing intervals between micturitions. Patients with OAB usually urinate 100 -150ml every time. The respective urine volume in a normal micturition is approximately 250-350ml. During the first days, the effort to inhibit micturition may seem to you torturing, but it will becomes easier over time. It is wise to fill in a 24-hour urinary diary every week, in order to have an objective evaluation of your progress. The aim is to limit micturition to 5-6 times every 24 hours (about 3-4 times/day). Re-education of the bladder is a hard process and takes time and effort. The results are better when you are monitored by your physician, who will provide advice and support.
Pelvic floor exercises
It has been observed that when tightening/ contracting pelvic floor muscles, we can temporarily inhibit bladder contraction and postpone micturition. Therefore, there are special pelvic floor exercises in which you can be trained by a specialized Physiotherapist. In some patients, OAB is combined with urinary incontinence. A trained Physiotherapist is able to teach you some exercises which 'teach' the pelvic floor muscles to retain the urethra and prevent the involuntary urine leakage. In this way, you can learn to control your incontinence.
Pharmacotherapy
If lifestyle changes and bladder re-education do not help, your Physician may administer some drugs to improve your symptoms. These pharmaceutical agents are called 'anticholinergics' and aim at relaxing the bladder so that it can receive higher quantity of urine. In some patients, symptoms may improve but not in every one. Also, the degree of improvement differs from person to person; and it is affected by the use of a different drug of the same category. You should take the drug for at least one month so that your physician will be able to evaluate its efficacy. Accordingly, s/he will modify the dose or replace it with another one. Also, the duration of the treatment is individualized depending on the case, but it usually lasts 3-6 months. However, it should be known that even though there is improvement with medication, after discontinuation of the treatment there will be recurrence of OAB symptoms in 2 out of 3 patients. It is better when pharmacotherapy is combined with a bladder re-education program, which reduces the chances of symptoms recurrence after drug discontinuation. The drugs have some side effects. The most common ones are xerostomia and constipation occurring in some patients. If any one of these occur, you should report it to your doctor so that s/he helps you to cope with it. Also, in case the drug does not help you or induces adverse events, your doctor may recommend another drug of the same category which may be proven more suitable for your case.
Surgical treatment
If the above treatments fail, your physician may recommend you some surgical intervention. These procedures are not simple and are performed only in a small number of patients with very intense symptoms. Surgical options are the following:
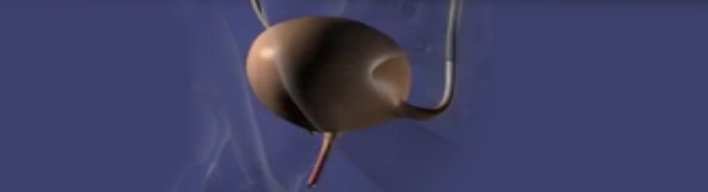
- Insertion of Neurostimulator. A special device is implanted in the spine, at the point where some nerves of the bladder arise from. The device sends electric signals to the bladder, for relaxing it.
- Augmentation Cystoplasty. When the bladder has low urine capacity, an intestinal part is resected (cut) and is sutured on the bladder like a patch. In this way, the bladder size increases and also increases the amount of urine that can be stored. When undergoing this surgical procedure, some patients may need to use single-use catheters for emptying the bladder (intermittent catheterizations).
- Urinary Diversion. The urine does not follow the normal pathway which is through the urinary bladder. Instead the urine is discharged through a sachet that is inserted in the abdomen.
Botox therapy
This is an alternative therapy instead of surgery. The therapy includes infusion of a neurotoxin, Botulinum Toxin A, into various sites of the bladder through the urethra, with the use of a special needle. In this way, the uncontrollable contractions of the detrusor muscle in the bladder are interrupted. The efficacy of the therapy lasts about 6-9 months and can be repeated. In some cases, though, there is a rick of the bladder not being able to void normally and the patient may then need to use single-use catheters (intermittent catheterization). This therapy is officially approved only for patients with multiple sclerosis and spinal cord injuries.